Osteoporosis is a very commonly seen condition among ageing population: it weakens bones, making them fragile and more likely to break. ReLiva physiotherapists who see geriatric patients across different Physiotherapy clinics in India report that fracture of wrist, spine and hip are most common due to osteoporosis but fracture of ribs, humerus (upper arm bone) and pelvis are not uncommon either.
Studies indicate the number of osteoporosis patients in India alone, at approximately 36 million (2013). Osteoporosis leads to more than 1.5million fractures each year. Statistical data shows that 1 out of 2 women older than 50 years have osteoporosis related fractures and 1 out of 3 men older than 75 years.
Our physiotherapists often get asked multiple questions related to orthopedic issues arising due to osteoporosis. We have compiled these questions raised by patients across different ReLiva Physiotherapy clinics. In this article, we attempt to answer most of these Frequently Asked Questions – FAQs on Osteoporosis.
Osteoporosis FAQs I Dos & Don’ts I Physiotherapy Treatment I Causes I Symptoms I Risk Factors I Prevention I Exercises
What Is Osteoporosis?
Osteoporosis (meaning porous bone) is a bone disease in which bone loss occurs, so that bones become weak and are more likely to break. It develops slowly over several years and is often only diagnosed when a minor fall or sudden impact causes a bone fracture. Without prevention or treatment, osteoporosis can progress without pain or symptoms until a bone breaks (fractures). Fractures from osteoporosis commonly occur in the hip, spine, ribs, and wrist.

What are the Do’s and Don’ts for managing Osteoporosis?
Here is a list of the most fundamental Dos and Don’ts in case you are dealing with Osteopenia and Osteoporosis:
Do’s for Osteoporosis patients:
- Include weight bearing exercise in your daily routine – They raise the heart rate enough to prove aerobic conditioning and ensure general health. You should target to walk 15 to 20 min, 3 to 4 times a week.
- Brisk walking is almost always the weight bearing exercise of choice for osteoporosis unless contraindicated (eg cardiac conditions, arthritis of lower extremities)
- Exercises should be increased gradually, until you reach your targeted duration of workout.
- Do not use inclination when using treadmill.
- Stick to low impact aerobic exercises. High impact aerobic exercises put too much stress on already weakened bone and should be avoided.
- Include high calcium diet
- Ensure exposure to sun, especially during morning hours.
Don’ts for Osteoporosis patients:
- Avoid running for patients with osteoporosis.
- Avoid rowing machines which cause vertebral compression fractures in those at risk.
- Avoid vigorous exercises accompanied with acute diet especially among young female. Young females should particularly understand that excessive exercise and consuming fewer calories than required for vigorous training will cause significant bone loss (athletic amenorrhea). Bone mineral loss in young female athletes with athletic amenorrhea of more than 6 months duration resembles that seen after menopause.
- Avoid high impact strenuous Patients who are not diagnosed with osteoporosis can perform some high impact exercises to prevent osteoporosis.
- Cut down on intake of tobacco and alcohol
What Causes Osteoporosis?
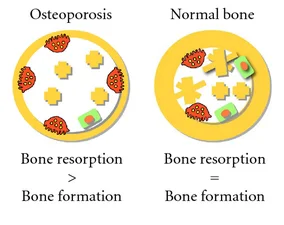
Bones may seem like hard and lifeless structures, but they are in fact living tissue. Bone is constantly broken down and remodeled (through a process called bony resorption) by our bodies, while new bone is simultaneously deposited. When bone is broken down faster than it is deposited, low bone mass or osteopenia occurs and the condition may aggravate eventually to cause osteoporosis.
Low bone mass -> Osteopenia -> Osteoporosis
How does Physiotherapy help in Osteoporosis?
Bones may seem like hard and lifeless structures, bones are more like muscle; bones are living tissues that respond to exercise by becoming stronger. Physiotherapy management for individuals with osteoporosis or even osteopenia will go hand-in-hand with the dietary intake to improve the bone strength. Physiotherapy management of osteoporosis will include a variety of exercises.
A physiotherapist may recommend certain exercises, such as those to strengthen the back and protect the spine from fractures. A physiotherapist may also recommend not performing certain exercises because exercise may put sudden or excessive strain on the bones.
At ReLiva, your physiotherapist will suggest you a plan of exercises based on your individual assessment of physical status and requirement.
Your physiotherapy plan of care for osteoporosis, will include some or all of the following:
- Weight bearing exercises
- Strengthening exercises
- Flexibility exercises
- Postural exercises
- Balance exercises
Who is likely to get Osteoporosis?
Generally, osteoporosis is less common in men than in women. This is true for several reasons.
- First, men have larger skeletons, meaning that they can usually afford to lose more bone before their bone strength becomes compromised.
- Second, their bone loss tends to start later in life and progresses more slowly.
- Third, they do not experience the rapid bone loss that affects women when their estrogen production drops as a result of menopause.
However, despite these differences, men are still at risk for osteoporosis.
What are the Risk Factors for Osteoporosis?
We can identify specific risk factors for Osteoporosis in two categories: Modifiable and non-modifiable
Modifiable risk factors for Osteoporosis:
- Hormone levels: Early menopause occurring naturally or surgical removal of ovaries can increase the likelihood of developing osteoporosis among women. Hormone replacement therapy (HRT) is usually the treatment choice.
- Diet: Low calcium and Vitamin D intake is harmful for bone health. It is important to watch-out for proper intake of calcium rich foods. A word of caution here: excessive consumption of protein and sodium may cause poor absorption of calcium.
- Exercise: Maintaining physically active lifestyle throughout life is important. Individuals who are inactive , immobilized or bedridden for a long time are at risk of osteoporosis.
- Lifestyle choices: smoking results in increased breakdown of exogenous estrogen, lower body weight and earlier menopause, all of which contribute to lower bone mineral density.Tobacco smoking inhibits osteoblastic activity leading to thinning of bone.
- Excessive alcohol intake: Too much of an alcohol use increases risk of bone loss due to poor nutrition and increased risk of falling.
Non modifiable risk factors for Osteoporosis:
- Gender: Women are more affected than men as they have thinner and lighter bones and lose bone mass rapidly after menopause.
- Age: Risk of osteoporosis increases with age
- Heredity: Those with a family history of fracture or osteoporosis are at an increased risk; the heritability of the fracture, as well as low bone mineral density, is relatively high, ranging from 25 to 80%. At least 30 genes are associated with the development of osteoporosis.
- Built: Small framed women and men are at higher risk than large and big boned persons. Incidence of osteoporosis is lower in overweight people.
- Ethnicity: While osteoporosis occurs in people from all ethnic groups, European or Asian ancestry predisposes for osteoporosis.
- Medical history: Those who have already had a fracture are at least twice as likely to have another fracture compared to someone of the same age and sex. Early menopause/hysterectomy is another predisposing factor.
How do I know if I have Osteoporosis?
Osteoporosis is known as a silent disease, as it does not usually cause any symptoms. Many people do not find out that they have osteoporosis until they have suffered a bone fracture.
Osteoporosis Signs and Symptoms:
Osteoporosis generally does not become clinically evident until fracture occurs. A few conditions / symptoms typically associated with osteoporosis include:
- Debilitating acute and chronic pain in the elderly is often attributed to fractures from osteoporosis and can lead to further disability and early mortality. These fractures may also be asymptomatic. The most common osteoporotic fractures are of the wrist, spine, shoulder and hip.
- The symptoms of a vertebral collapse (“compression fracture“) are sudden back pain, often with
- radicular (shooting pain due to nerve root compression) and
- rarely with spinal cord compression or cauda equina syndrome.
- Multiple vertebral fractures lead to :
- a stooped posture,
- loss of height,
- chronic pain, and
- resultant reduction in mobility
How can I prevent Osteoporosis?
Whether you are young or old, you can remain careful about a few things to prevent onset of osteoporosis, which include:
- Food Intake: Include food rich in calcium and Vitamin D in your diet. Calcium plays an important role in maintaining bone health. Vitamin D on the other hand, helps the small intestine to absorb calcium. It also slows the removal of calcium from the body by the kidneys. In other words, calcium and vitamin D work together to help maintain bone health. Vitamin D is manufactured in the skin following direct exposure to sunlight. Many people are able to get enough sun exposure in their day-to-day lives and do not need vitamin D supplementation. Foods rich in calcium include milk, cheese, tofu, and broccoli.
- Exercise: Like muscle, bone is living tissue that becomes bigger, denser, and strong with consistent exercise. To maintain and increase bone density and strength, both weight-bearing exercises and resistance exercises are helpful. This will also help in preventing falls.
- Lifestyle changes: Maintaining a normal body mass index (body weight proportional to height and frame size) and avoiding tobacco and alcohol use are key factors to consider.
Maintaining bone health in elderly population is particularly important as there is typically a decline in bone mass with age.
How Is Osteoporosis Detected?
Unfortunately, many people do not know they have osteoporosis until they experience a broken bone. By that time, bones are already weak. However, osteoporosis can be prevented or delayed by early detection and treatment.
- Specialized tests called bone density tests can measure bone density (solidness) in various sites of the body. These tests are quick (taking less than 15 minutes), painless, and noninvasive and are extremely helpful in screening for and making a diagnosis of osteoporosis. This bone density measurement provides a quantitative assessment, called a T-score, which can be used for diagnosis and monitoring during management. A bone density test can detect osteoporosis before a fracture occurs and can predict your chances of having a broken bone in the future.
- A dual-energy X-ray absorptiometry (DXA) scan of bone mineral density (BMD) can determine your rate of bone loss and/or be used to monitor the effects of treatment.
What is the treatment for Osteoporosis?
At the present time, it is generally agreed that all people can reduce their risk & impact of developing osteoporosis through the following strategies:
Osteoporosis Treatment:
- Calcium and Vitamin D supplements: While calcium alone cannot prevent or cure osteoporosis, it plays an important role in maintaining bone health by increasing bone mineral density and reduce risk of fractures. Vitamin D is essential for calcium absorption. Include food rich in calcium and Vitamin D in your diet. In acute conditions, your doctor may prescribe you supplements to recover quickly.
- Hormone Replacement Therapy (HRT): It is an established treatment for osteoporosis. It helps maintain bone mass in post menopausal women.
- Exercise: Resistance and impact exercise are most beneficial to bones. It promotes high peak bone mass during childhood and adolescence. It slows down decline in bone mineral density (BMD) when performed later in life provided Calcium and Vitamin D intakes are adequate. Ask your physiotherapist to design an exercise program that is suitable for your bone condition and body.
What kind of exercises help in the treatment of Osteoporosis?
Exercise is an important part of an osteoporosis treatment program. Although bones may seem like hard and lifeless structures, bones are more like muscle; bones are living tissues that respond to exercise by becoming stronger. Exercise improves bone health. An additional benefit is that exercise also increases muscle strength, coordination, and balance and leads to better overall health. Exercise is good for people with osteoporosis. However, discuss any exercise program with a doctor or physiotherapist.
Your exercise program should include exercises from all of the three categories:
1. Weight bearing exercises
Regularly performing weight-bearing exercise (exercise that works against gravity) has been shown to help maintain and build up bone mass. Weight-bearing exercises include walking, hiking, jogging, climbing stairs, playing tennis, and dancing.
2. Strengthening and Flexibility exercises
One should do resistance exercises to build muscle mass and strengthen bone. These activities include weight lifting, such as using free weights and weight machines found at gyms and health clubs. Strengthening should involve all major groups of muscles. The added benefit of these exercise are stronger muscles and better balance and coordination, which can also help prevent falls.
3. Postural and Balance exercises
Falls are a serious worry in anyone with weakened bones (such as from osteoporosis) because even a minor fall can cause a serious injury or even permanent disability. Improving postural control is important to reduce the risk for falls.
Specific postural and balance exercises can help improve the individual’s overall physical function and postural control to minimize aches and pains and eventually to further reduce the risk of fall.

When Does Osteoporosis Occur?
Osteoporosis can occur at any age. However, it is more common in people older than 50 years of age, and the older a person is, the greater the risk is of osteoporosis. This is because during childhood and teenage years, new bone is generally added faster than old bone is removed.
This is the time when a diet rich in calcium, phosphate, and vitamin D is important. As a result, bones become larger, heavier, and denser. Maximum bone density and strength is reached by 20-25 years of age. The density and strength of the bones is fairly stable from 25-45 years of age. A slight loss of bone density begins to occur after age 30 because bone slowly begins to break down (a process called resorption) faster than new bone is formed.
For women, bone loss is fastest in the first few years after menopause, but it continues gradually into the postmenopausal years. As bone density loss occurs, osteoporosis can develop. This process is slower by 10 years in men.
Are there types of Osteoporosis? What causes them?
Technically speaking, there are 2 different categories of osteoporosis:
- Primary Osteoporosis: Primary osteoporosis is the most common form and can occur among both men and women.
- Type 1 osteoporosis, which usually follows menopause in women.
- Age-related osteoporosis, which occurs later in life – more so among men due to decreased testosterone production.
- Secondary Osteoporosis: Secondary osteoporosis can occur in people who either take medications or suffer from diseases that can cause decreased bone density. Possible causes of secondary Osteoporosis are:
- Anti-seizure medication
- Excessive thyroid hormone medication
- Gonadotropin hormone
- Certain anti-cancer drugs
- Inflammatory disorders treated by steroids eg asthma, lupus, rheumatoid arthritis
- Bone marrow disorders
- Low sex hormone levels – Among women, a result of excessive exercise (amenorrhea) or eating disorder that decrease estrogen production or premature menopause.
What Lifestyle Changes Affect People With Osteoporosis?
Quit smoking
Smoking is bad for the bones as well as for the heart, lungs, stomach, skin, teeth, and hair. Women who smoke have lower estrogen levels compared with women who do not smoke. Lower estrogen levels result in decreased bone mass. Smokers may also absorb less calcium from their diets, and calcium is necessary for strong bones. Finally, women who smoke and choose hormone replacement therapy after menopause may require higher doses of hormones and have more complication
Limit alcohol intake
Regular consumption of 2-3 ounces of alcohol a day may be damaging to bones, even in young women and men. Heavy drinkers are more likely to have bone loss and fractures. This is related to both poor nutrition and increased risk of falling. However, some evidence indicates that moderate alcohol intake may have beneficial effects on bone mass.
Psychological and Practical Support for People With Osteoporosis
No cure exists for osteoporosis, but effective treatment plans are available. Support networks are important to successful treatment. Information on preventing falls and maintaining a healthy diet and exercise routine is widely available. Physical rehabilitation after fractures can be a long process, and psychological and practical support is important. Your physiotherapist can help in rehab and also provide practical advice, including strategies to prevent falls.
Now that you understand the causes, prevention and management of Osteoporosis, we hope that you will take due care to prevent its onset. If osteoporosis has already made a silent entry, then you can surely manage it better with diet, supplements and exercises with a physiotherapist.
If you need help with an exercise regime that will suit your specific body and bone condition, then call us at +91 992099 1584 and we will connect you with a physiotherapist near you to get you started.
This article is based on the inputs from Dr Suveda Kothari (PT). Dr Suveda is a senior physiotherapist at ReLiva with years of experience, helping patients in their recovery.
We provide Physiotherapy services at our fully equipped clinics in 15+cities in India. Find a physiotherapy clinic near you
Need PHYSIOTHERAPY?
ReLiva is there
Related Reading:
Fracture : Don’t leave it half healed
Understanding Spondylosis VS Spondylitis





